Introduction – A Link Many Don’t See Coming
When people think about sleep apnea, they often picture loud snoring, restless nights, and constant fatigue.
When they think about diabetes, they imagine blood sugar checks, dietary restrictions, and insulin.
At first glance, these two conditions may seem unrelated — one affects sleep and breathing, the other affects blood sugar regulation.
But growing research shows a strong connection between sleep apnea and type 2 diabetes, creating a health partnership that can make each condition harder to manage if left untreated.
Understanding this hidden link can be life-changing. By treating one, you may improve the other — and reclaim both your nights and your days.
What Exactly Is Sleep Apnea?
Sleep apnea is a disorder where breathing repeatedly stops and starts during sleep. The most common form, obstructive sleep apnea (OSA), happens when the muscles in the throat relax too much, blocking the airway. This forces the brain to wake the body just enough to restart breathing, often without you even realizing it.
This disruption prevents deep, restorative sleep, leading to fatigue, mood changes, and — as science now shows — greater risk for metabolic issues like diabetes.
See more: A Complete Guide to Buying CPAP Masks Online: Tips for Finding the Best Fit
The Connection Between Sleep Apnea and Diabetes
Research suggests that up to 80% of people with type 2 diabetes also have sleep apnea, many without knowing it. Here’s why they’re linked:
- Oxygen Drops and Stress Hormones
Each time your breathing pauses, oxygen levels fall. This triggers a stress response, releasing hormones like cortisol and adrenaline, which can raise blood sugar. - Poor Sleep Quality
Sleep deprivation affects insulin sensitivity, making it harder for the body to manage glucose. - Weight and Inflammation
Obesity is a major risk factor for both conditions. Inflammation from poor sleep can further damage insulin-producing cells.
Example:
Mark, 52, was struggling to manage his blood sugar despite medication. After his wife noticed loud snoring and gasping during the night, he was diagnosed with sleep apnea. Once treated, his morning glucose readings improved significantly.
Causes of Sleep Apnea
Sleep apnea isn’t caused by a single factor — it’s usually the result of a combination of physical traits, lifestyle habits, and health conditions.
1. Physical Factors
- Narrow airway or enlarged tonsils
- Thick neck circumference
- Receding chin or jaw structure
2. Lifestyle Factors
- Excess weight, especially around the neck and abdomen
- Smoking, which inflames airway tissues
- Alcohol consumption before bed, which relaxes throat muscles
3. Health-Related Triggers
- Chronic nasal congestion from allergies or sinus problems
- Hormonal changes, such as during menopause
- Neurological issues (for central sleep apnea)
Symptoms to Watch For
Because sleep apnea happens during sleep, many people aren’t aware they have it. Sometimes, it’s a partner who notices the signs first.
Obvious Symptoms
- Loud, chronic snoring
- Gasping or choking during sleep
- Pauses in breathing
- Morning headaches
- Waking up with a dry mouth
Subtle Symptoms
These are especially important because they often go overlooked — yet they have a huge impact on daily life and diabetes management:
- Daytime fatigue or sleepiness
- Trouble concentrating or remembering details
- Irritability or mood swings
- Difficulty losing weight despite diet and exercise
- Worsening blood sugar control despite medication
Scenario:
Lisa, a teacher with type 2 diabetes, found herself forgetting lesson plans and snapping at students. She thought it was stress, but a sleep study revealed severe sleep apnea. Treatment not only improved her mood but also stabilized her glucose levels.

How Sleep Apnea Affects Blood Sugar Control
The relationship between these two conditions is a two-way street:
- Sleep apnea makes diabetes worse by increasing insulin resistance.
- Diabetes can worsen sleep apnea by causing nerve damage that affects airway control or increasing inflammation.
Over time, untreated sleep apnea can lead to higher A1C levels, making diabetes harder to manage and increasing the risk of complications like heart disease and kidney damage.
Treatment Options – Improving Sleep and Blood Sugar
The good news: treating sleep apnea often leads to better diabetes management. Here’s what works.
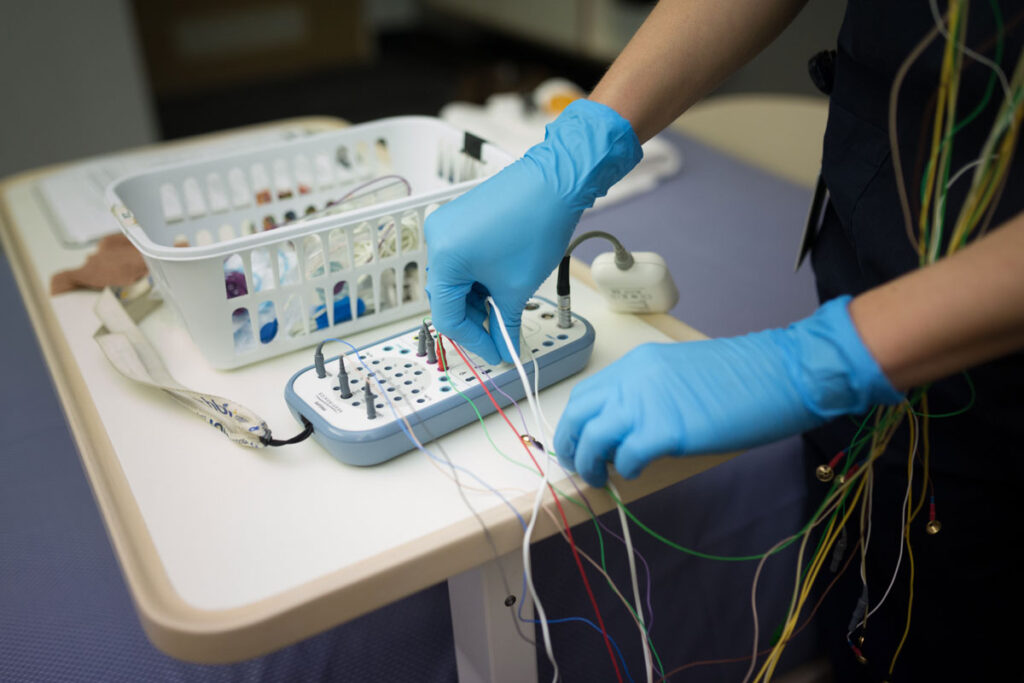
1. CPAP Therapy
The gold standard for moderate to severe sleep apnea, Continuous Positive Airway Pressure (CPAP) machines keep the airway open with a gentle flow of air.
Benefits for Diabetes:
- Improves insulin sensitivity
- Reduces morning blood sugar spikes
- Boosts energy for exercise and daily activities
Real-Life Impact:
After starting CPAP, Daniel not only stopped nodding off at his desk but also saw his A1C drop from 8.2% to 7.0% within six months.
2. Oral Appliances
Custom-fitted mouthpieces reposition the jaw or tongue to keep the airway clear.
Best For:
Mild to moderate sleep apnea or people who can’t tolerate CPAP.
3. Weight Management
Even a 5–10% weight loss can reduce airway blockage and improve both sleep apnea and blood sugar control.
Tips:
- Focus on high-fiber, nutrient-dense foods.
- Incorporate regular, moderate-intensity exercise.
- Avoid late-night heavy meals.
4. Positional Therapy
Training yourself to sleep on your side (instead of your back) can help keep the airway open.
5. Surgery
For structural issues like enlarged tonsils, deviated septum, or severe jaw misalignment, surgical options may provide relief.
6. Lifestyle Adjustments
- Avoid alcohol within three hours of bedtime.
- Quit smoking to reduce airway inflammation.
- Maintain a consistent sleep schedule to help regulate hormones that affect glucose.
Why Treating Sleep Apnea Matters Beyond Sleep
When sleep apnea is addressed, people often notice:
- More consistent energy levels
- Better mood and mental clarity
- Improved ability to exercise
- Lower blood pressure
- Better long-term diabetes control
It’s not just about snoring less — it’s about reducing the strain on your heart, brain, and metabolism.
Conclusion – Don’t Overlook the Connection
Sleep apnea and diabetes share more than a passing link — they can fuel each other in ways that damage your health and quality of life. The good news is that with proper diagnosis and treatment, you can break this cycle.
If you have diabetes and struggle with fatigue, poor sleep, or trouble focusing, it’s worth getting evaluated for sleep apnea. Likewise, if you’ve been diagnosed with sleep apnea, ask your doctor about screening for diabetes.
Better sleep can mean better blood sugar — and better overall health. And that’s a connection worth waking up to.